014: Eating Right with Migraines, with Stephanie Weaver MPH
Leave us a Rating & Review Here
Most doctors get absolutely no nutrition training in Med School. We sort of expect them to know more about it than they actually do.
Stephanie Weaver MPHAuthor, The Migraine Relief Plan
SUMMARY
Food expert and author of The Migraine Relief Plan Stephanie Weaver MPH examines many of our assumptions about food and migraine that simply aren’t based in evidence. She offers encouragement to anyone who wants to eat right for migraines on choosing foods that can reduce painful attacks. She considers food to be just part of the “medicine” for effective migraine prevention.
3 KEY POINTS
- Food sensitivities are a very personal thing. Just because someone else is sensitive to soy or gluten or dairy doesn’t mean everyone is.
- There is no formal evidence for the low-tyramine diet recommended by many headache doctors, just patient-reported sensitivities gathered by clinicians.
- Given the lack of formal research on nutrition for migraine, the best way to test any diet for migraine like Paleo, Ketogenic, Sugar-Free, Low Tyramine is methodical self-testing and tracking of attack frequency and intensity over a period of time.
Show Notes
Stephanie W.: Yeast-free is trying to eliminate tyramine. Sugar-free is eliminating the inflammation that sugar can bring, and gluten-free is the same. You’re eliminating the potential inflammation that can create the environment in your brain that might make you more likely to trigger into a migraine attack.

Stephanie Weaver
Paula Dumas: Have you tried to change the way you eat due to migraine? Many of us have seen the extensive list of migraine-triggering foods, which is just long enough to bring on a full-blown anxiety attack, and that is not helpful. But if you’re curious about all the migraine diets out there like Paleo, ketogenic, yeast-free, gluten-free, sugar-free, and so on, do not miss today’s guest.
She’s a wellness coach and diet expert who also struggles with migraine. She’s here to help us sort through the pros and cons of different diets and make it simple to eat well. We’ll be back to meet her right after this.
Paula Dumas: Stephanie Weaver is the author of The Migraine Relief Plan, a gentle eight-week transition to better eating, fewer headaches, and optimal health. Stephanie has a master’s degree in public health and nutrition education and is also a certified wellness coach. In addition to her extensive training, Stephanie is also a professional wellness speaker, food photographer, recipe developer, and blogger.
Stephanie, welcome to Migraine Again.
Stephanie W.: Thanks so much for having me, Paula.
Paula Dumas: We are delighted to have you here, and food is one of our favorite topics to dive into. My migraine was diagnosed at 24, just a few years ago, and shortly after I saw the doctor I went to this place that we used to call a library. Remember those places?
Stephanie W.: Yes, I do.
Paula Dumas: I went to the library and I checked out a book on migraine diets and I started my first attempt to control it with food.
Your migraine attacks began later in life, which is kind of unusual. What’s been your experience with diet in terms of changing your own health?
Stephanie W.: I have changed my diet for health reasons, I think seven or eight times over the course of my lifetime. I’ve had issues with allergies, I’ve gone vegetarian, I went vegan for a while, I ended up going gluten-free, so I have a lot of experience with changing my diet for health reasons. Now that I know what my migraine pattern is, I actually have had migraines my whole life, they were just quite atypical and so I didn’t get diagnosed until I was 53. I’m pretty sure I had abdominal migraines as a kid, and I know I had what I thought were weather headaches, and even though
I saw different doctors and we tried different things, no one ever told me I was having migraines. Because I didn’t have aura and they weren’t incredibly disabling, I just kept on going with my life. It wasn’t until I started having vertigo that I actually got diagnosed.
Paula Dumas: It was the vertigo that got you the diagnosis — that’s crazy.
Stephanie W.: Yes, it is crazy. That was I think because post-menopause my symptoms shifted. Of course we never know because it is an unpredictable condition that we have, but that’s my guess, is that with my changing hormonal pattern the migraines started showing up as vertigo. Of course that was something that I couldn’t really ignore. I had to go find out what was going on.
But I do have a really strong belief, and I guess it would be a bias (but I think in a good way), that food is an enormous part of our health and our wellness. That’s kind of how I approached this, as well as my doctor. The first thing he did was he gave me the “migraine diet sheet” which is the low-tyramine diet. That was what I went home with, and because I had this background in food and changing recipes and I’d been doing this for a long time, that was my interest as well, was what can I do to help myself feel better? I think a lot of people like yourself, we have that we want to feel more in control and so we’re looking for answers, and we do eat three to five or more times a day, so food seems like a natural place to start as well.
Paula Dumas: Yeah, some of the doctors that we work with and who I’ve interviewed for the Migraine World Summit will say, “Why is food such a huge part of your content the EAT channel on Migraine Again?” I said, “Because we kind of think that food can be medicine, and it can be a big contributor to your wellness or how you feel, negative or positive.” It seems like many of the people in our community have the same orientation to that. Not everybody does, but many of them believe that food is a choice that is within their control every day.
Stephanie W.: Absolutely.
Paula Dumas: Learning to make better choices will in the long run pay out. Now, what made you want to empower others using diet as a catalyst for this kind of positive change in their health?
Stephanie W.: I have a master’s of public health, as you mentioned, in nutrition education and so I’ve always been interested in nutrition. I started my food blog a little over seven years ago to try to help people who had to be on special diets for health reasons feel like they had great choices, so that it wasn’t about want and lack and “this isn’t as good as …”. Food can be, if you’re creative, food can be an amazing part of your life. Even if you’re gluten-free or you’re not eating sugar or you choose to go completely plant-based, you shouldn’t have to feel like, “Wow, I am eating less than other people.” It was a natural place for me to come in, so I came in with that mindset. I was working on my food blog, I was developing recipes, I’m given this diet list, and so of course I’m going to start researching.
Even though I’m not a registered dietician, but I have a lot of nutrition background, and I had never heard of tyramine which is an amino acid breakdown product, so tyrosine is the amino acid, it’s a naturally occurring substance in food, I’d actually never heard of it. Apparently this was what was causing my migraines, according to this three page handout, which of course we know is not true. There’s many things that cause migraine, but that was where I started. Then as soon as I started looking into it, I realized wow, there’s a whole lot of not information that’s available. There’s conflicting information. Every list I looked at was different and so I was very confused, but I kept working at it because I did feel like I’ve seen good results in the past when I had chronic fatigue syndrome and I really shifted my diet, that really helped me. So I knew that there could be a potential shift. I wasn’t expecting to cure myself or anything like that, and I certainly don’t promise that to anyone, but I definitely have that bias.
I think some MDs have that bias and some don’t. You kind of mentioned that earlier. If you talk to integrative medicine doctors, functional medicine doctors, they’re all about diet and lifestyle, whereas the allopathic doctors that haven’t gone into that level of training maybe, they don’t necessarily have that perspective.
Paula Dumas: Most doctors get no nutrition training in med school.
Stephanie W.: Correct.
Paula Dumas: So that’s their orientation. Nor in continuing education.
Stephanie W.: Right, because they’re choosing to keep up their continuing medical education hours in neurology or whatever their specialty is, and I totally understand that. We sort of expect that they’re going to know more about this than they actually do, and so that’s something that people should be aware of, is that maybe your doctor doesn’t know that much about nutrition. Mine said to me, “I want you to tell me everything you’re learning because you already probably know more than I do and I want you to fill me in.” That was a great partnership for me.
Paula Dumas: That is good. That’s great that he or she was humble enough to welcome that from you.
Stephanie W.: Yes, it was awesome.
Paula Dumas: You know, I’ve tried a few diets to control my migraine attacks. I did five weeks on a yeast-free diet. That was the first one I tried. Felt amazing. It was incredibly effective until it stopped working. Then I tried eliminating all the trigger foods in the Heal Your Headache book, with no relief. I tried two years of going gluten-free, which helped my digestion really well, but it didn’t change the frequency or intensity of my migraine attacks. Then finally I tried tracking my triggers using an app called Curelator for 90 days, and I removed the offending foods. That really helped me make some progress. Curiously, one of the things it identified was that when I consumed tyramines it was actually a helpful thing instead of what many people experience, which is that tyramines are a negative thing. That’s just another way of seeing how each of us are very, very different.
Stephanie W.: That’s fascinating.
Paula Dumas: It is fascinating. What does the evidence say about using diet to help improve health conditions such as migraine?
Stephanie W.: That was an awesome overview of the challenges of diet and a condition like migraine, which is unpredictable and it has multiple factors. We know it’s a neurobiological condition. There’s a number of theories. Sometimes they seem to go in and out of favor. For a while I think people really focused on food triggers and that food was a big piece of it. Now, we were both just at the American Headache Society and I kind of felt like the pendulum had swung away from that and people were saying, “Triggers are really all about the prodrome and you’re not really actually causing the migraine. It’s actually already started and you just have a food craving.” That’s entirely possible. We don’t know, because we just do not know.
What I can say is that when I looked into the [migraine] diet sheet that I was given, I could not find how it was developed, and I did a lot of research. I contacted every organization that had a diet sheet on their website, and no one could tell me where the list came from or what research it was based upon. So that’s that. That’s a question mark. Where did that come from and then how was it developed?
There have been a few studies related to diet and migraine. Usually they’re pretty small. There was one in Turkey that was 30 subjects, and what they actually did which was very interesting was they tested them for food allergies, and then they would have a period of time where they were told not to eat certain foods and then they would switch over, and nobody knew. The doctors didn’t know and the patients didn’t know what foods they actually had tested allergic to. Of course everybody tested allergic to different foods. This is, I think, what’s so fascinating and challenging about this, is that every one of us is different. For what may work for you, like eating avocados, is not going to be helpful for someone else. That’s I think where the frustration comes in of how do we figure this out in a way that doesn’t make us completely nuts?
Then you have the members of a study on the low fat vegan diet that Center for Science in the Public Interest did, that did show a little bit of improvement, but when I talked to the principal investigator on that study, I felt that there … Well, there was certainly bias going in because that’s their position, that everybody should be on a low fat vegan diet. I’m not criticizing that, but we all have to understand that there’s always going to be bias within the researchers. They’re trying to prove something they already think might be the case.
The one thing I wanted to talk about is the anecdotal evidence, which is your personal experience or a person’s personal experience. You found that avocados actually helped you, and you did that in a really systematic way. It might be problematic though if you then put on your website, “Hey, avocados are the cure for migraines,” because they may not be helpful for everyone. That’s what I would call anecdotal evidence, like one person or a couple people.
Then there’s clinical practice, and I think that you mentioned the Heal Your Headache book, which is the best selling headache book on Amazon, so a lot of people have bought it and read it and tried it. My guess is that as many people found it helpful as didn’t find it helpful, because we’re all so different. But what is interesting about his dietary list is that it was worked on over the course of 30 years of his clinical practice with patients. For me, even though it’s not a scientific study, that’s valuable. He worked with patients over 30 years and developed this list and took some things off and put some things on based on what his patients were telling him. Even though there’s other things in his book that are problematic and people hate his book, love his book, whatever, I think that the value of that 30 years of clinical practice is an interesting piece for people to understand.
Then the third thing would be a randomized scientific trial where you have a bunch of people and they’re randomized into two groups and they test one type of diet perhaps, and then the other people don’t have that and maybe they switch them. But it’s very expensive to do. It’s very hard to do, and it’s tough because just imagine, unless you’re going to send meal kits to everyone and they’re never going to stray from what you’re giving them, it’s very expensive to do dietary work. I worked on a study when I first got out of public health school, and even just getting people to register how much of a particular food they ate is really hard.
I don’t think we’re ever going to have a definitive dietary study. I really wish we did. I would love to have someone have done that, and then I wouldn’t have had to write a book and would have said, “Okay, this is the way to go.” But what I found was that at least having a systematic approach to trying food I think is helpful, and then we do know based on population studies that certain kinds of ways of eating are helpful. We know that the standard American diet, which is very high in processed foods and packaged foods, has been problematic for people for a long time, and every time it’s introduced somewhere to a new population, you start to see increases in obesity and diabetes and some other issues. So we do know that.
We do know that people that eat the Mediterranean style diet seem to have better health outcomes overall. There’s blue zones, there’s five blue zones around the world that are very much very health-oriented places where people live a really long time and seem to have lower incidence of some of these illnesses, and they tend to eat all whole foods, primarily plant-based, a small amount of animal protein, and then there’s other factors involved as well.
We do know some broad strokes things about nutrition. The challenge is that we don’t have any really great studies that definitively prove one way or another what kind of foods you can eat to prevent a migraine.
Paula Dumas: Yeah. The evidence is a little bit thin, and so your own personal trial and error is probably the best approach, and giving it enough time, I suppose, to make sure that it works is really, really key. Thanks for that wrap up on the evidence. We’ll talk about some of the specific diets a little bit later.
There’s been a lot of buzz about salt as a treatment for migraine on social media. Based on the evidence that you’ve seen, is salt good or bad for people with migraine?
(CONTINUED) …
For the Complete Transcript Click Here
Enjoying the Podcast?
Leave An iTunes Rating & Review HereRESOURCES
- Stephanie Weaver – Facebook
- The Migraine Relief Plan: An 8-Week Transition to Better Eating, Fewer Headaches, and Optimal Health – Amazon.com
Migraine Again Articles
The Migraine World Summit
ABOUT OUR ADVERTISERS (Interested in becoming an advertiser?)
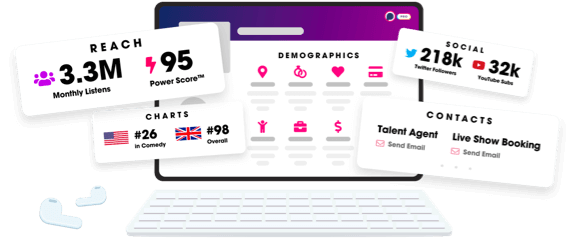
Unlock more with Podchaser Pro
- Audience Insights
- Contact Information
- Demographics
- Charts
- Sponsor History
- and More!
- Account
- Register
- Log In
- Find Friends
- Resources
- Help Center
- Blog
- API
Podchaser is the ultimate destination for podcast data, search, and discovery. Learn More
- © 2024 Podchaser, Inc.
- Privacy Policy
- Terms of Service
- Contact Us
